PrEP: NHS 'must urgently offer' HIV breakthrough nationwide as study shows infections cut 25% in a year
'Unacceptable' that PrEP provision in England is capped when there are no limits in other UK nations, National Aids Trust chief says
HIV/AIDs charities have called for the NHS to immediately commit to a national rollout of a breakthrough preventative treatment after results from an Australian trial showed it cut new transmissions by 25 per cent in a year.
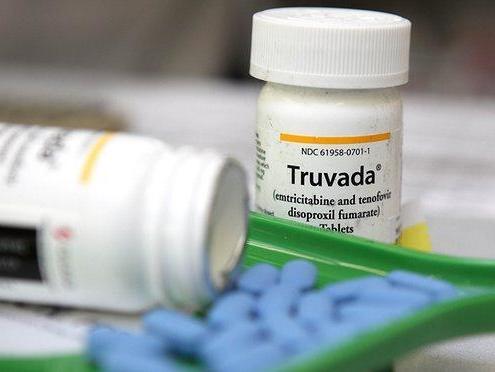
Research published in The Lancet medical journal on Wednesday has demonstrated the rapid effectiveness of pre-exposure prophylaxis (PrEP) treatment with the drug Truvada in a real world setting.
In the 12 months after the PrEP roll out in 2016, new HIV diagnoses among men who have sex with men in the Australian state of New South Wales fell to their lowest levels since recording began.
In trials, the daily medication is up to 99 per cent effective at preventing HIV taking hold in the body when its is transmitted during sex or through contaminated needles. It works by blocking a crucial enzyme that the human immunodeficiency virus needs to create copies of itself.
The NHS is currently running its own three year assessment of Truvada PrEP to assess its cost effectiveness and it has already expanded the number of people being enrolled beyond the 10,000 initially planned.
However, the National AIDS Trust (NAT) has said that people are being put at risk of infection because they cannot access the trial and the scheme should be rolled out nationwide – particularly as a patent ruling last month has meant its costs have fallen significantly.
Deborah Gold, chief executive, NAT, said in light of the increasing body of research on PrEP’s benefits it is “completely unacceptable for people in need of PrEP to be denied it”.
“This news highlights the incredible potential of PrEP to [help] finally reverse the HIV epidemic in any country,” she added.
“As it stands, England is the only UK nation with a capped provision of PrEP. NHS England and local authorities must urgently agree a national PrEP programme to start as soon as possible in 2019, and must ensure that anyone in need of PrEP can access it.”
The NAT also wants more work to be done to recruit women, trans people and other at risk groups such as migrant communities from countries with high levels of HIV/AIDs.
The Lancet study reports that 221 men in the state were diagnosed with HIV in the 12 months after the trial, a fall of 25 per cent from the 295 HIV diagnoses in the 12 months prior.
Of the 3,069 participants who received the drug for the trial – and who returned for testing 12 months later – there were only two HIV diagnoses.
Both these men reported that they had not stuck to taking the daily dose of Truvada, which undermines its effectiveness. But even with these cases, the new diagnosis rate was still 200 times lower than the infection rate in the general population of gay men.
mothers2mothers helping to educate families dealing with HIV diagnosis
Show all 9Declines in new infections went as low as 50 per cent in suburbs of Sydney with the largest proportion of gay residents.
“Our results support the population-level effectiveness of PrEP one year after rapid PrEP implementation at scale,” says Professor Andrew Grulich, from the Kirby Institute at UNSW Sydney, which led the study.
“PrEP is a highly effective preventative approach when implemented alongside high levels of HIV testing and treatment. Roll-out should be prioritised as a crucial component of HIV prevention in epidemics predominantly affecting men who have sex with men.”
An NHS England spokesperson said: “While it would be wrong to prejudge the PrEP Impact trial, it is already expanding with the number of places available increasing this year by 3,000 to 13,000.
“The NHS will look at evidence from the trial to expand prevention services in the most effective way.”
Subscribe to Independent Premium to bookmark this article
Want to bookmark your favourite articles and stories to read or reference later? Start your Independent Premium subscription today.

Join our commenting forum
Join thought-provoking conversations, follow other Independent readers and see their replies