People living with HIV can safely use checkpoint inhibitors, a type of immunotherapy that unleashes T-cell activity against cancer, according to study results presented at the American Society of Clinical Oncology (ASCO) annual meeting this week in Chicago.
Researchers reported that the PD-1 checkpoint blocker Keytruda (pembrolizumab) and the PD-L1 blocker Imfinzi (durvalumab) were safe and well tolerated in HIV-positive people with various types of cancer. Response rates were in line with those seen in HIV-negative people.
As people with HIV live longer thanks to effective antiretroviral therapy, non-AIDS cancers have become a leading cause of illness and death. And while the three AIDS-defining cancers—Kaposi sarcoma (KS), non–Hodgkin lymphoma (NHL) and cervical cancer—have decreased dramatically since the mid-1990s, many HIV-positive people still develop them.
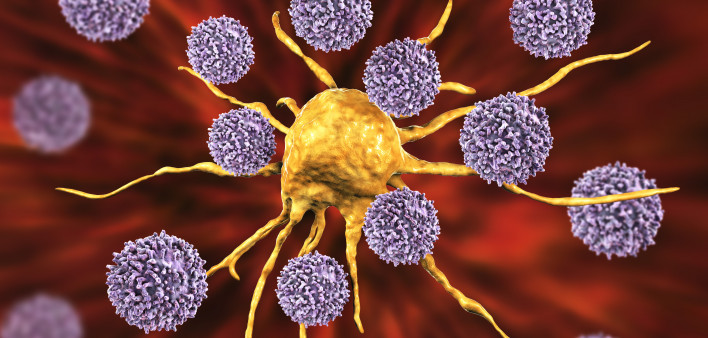
Immunotherapy, which helps the immune system fight cancer, offers a promising new approach to treatment. PD-1 is a checkpoint protein on T cells that helps regulate immune function. Some tumors can hijack PD-1 to turn off immune responses against them, and drugs that block the interaction between PD-1 and its binding partner, known as PD-L1, can release the brakes and restore T-cell activity.
To date, there has been limited research on immunotherapy for HIV-positive people with cancer, as they have generally been excluded from oncology clinical trials. In part, this has been attributed to concerns about worse side effects and interactions between cancer drugs and antiretrovirals. In addition, some experts feared that this type of treatment could compromise HIV control, though small studies of checkpoint inhibitors in HIV cure research suggest they may actually help suppress the virus and possibly even reduce the latent viral reservoir.
Fortunately, this is changing. Last November, at the urging of ASCO and Friends of Cancer Research, the National Cancer Institute and the Food and Drug Administration expanded trial eligibility criteria to allow people with certain coexisting conditions, including HIV. Also last year, the National Comprehensive Cancer Network issued new guidelines recommending that clinicians should offer cancer treatment to most people with HIV just as they would for those who are HIV negative.
Some retrospective studies have suggested that checkpoint inhibitors are safe and effective for people with HIV and cancer. But these analyses have looked back at cases of HIV-positive people who happened to receive these drugs in real-world clinical practice. The studies presented at ASCO are among the first prospective cancer treatment trials to specifically enroll and follow people with HIV.
Keytruda
In the first study, sponsored by the National Cancer Institute, Thomas Uldrick, MD, of the Fred Hutchinson Cancer Research Center in Seattle, and colleagues evaluated whether Keytruda is safe for people living with HIV and advanced cancer across a range of CD4 cell counts. Results were simultaneously published in JAMA Oncology.
This early analysis from the ongoing Phase I trial included 30 people with HIV and various advanced cancers at seven Cancer Immunotherapy Trials Network sites between April 2016 and March 2018. All but two were men, 60% were white and the median age was 57 (age range 39 to 77).
Participants had to be on antiretroviral therapy for at least four weeks and had a viral load less than 200 copies. They were required to have a CD4 count of at least 100 cells. Six had 100 to 199 cells, 12 had 200 to 350 cells and 12 had more than 350 cells. People with active hepatitis B or C coinfection, a history of autoimmune diseases or recent use of immunosuppressive therapies or other cancer drugs were excluded.
The participants had relapsed or refractory (nonresponsive) cancers and were not eligible for other standard therapies. Eleven had AIDS-defining cancers: six with KS and five with NHL. Interestingly, four of these had CD4 counts of 200 to 350 and six had counts over 350. The remaining 19 had non-AIDS cancers, including six with anal cancer, three with metastatic skin cancer, two with bladder cancer and one each with non-small-cell lung cancer, sarcomatoid lung cancer, liver cancer, pancreatic cancer, prostate cancer, tonsil cancer, adenoid cystic carcinoma and cholangiocarcinoma.
Everyone in this open-label trial was treated with Keytruda administered as a 200-milligram intravenous infusion every three weeks for up to two years or until they experienced cancer progression or unacceptable side effects. They also continued taking antiretrovirals throughout the study.
HIV remained suppressed in all participants. CD4 counts increased by a median of 19 cells overall, but this rose to a 152-cell gain among those with stable disease for at least six months. However, neither difference was statistically significant, meaning they could have been driven by chance.
One person with lung cancer experienced a complete response, or full remission; two people with NHL had partial responses. Two patients experienced an unusual type of paradoxical lymphoma response sometimes seen with immunotherapy. Two people with KS had stable disease, meaning no further cancer progression, for six months or more, and 13 others had stable disease for less than six months at the time of the analysis. Uldrick reported that one person with liver cancer that had spread to the bones did not meet partial response criteria but had reduced pain and improved biomarkers lasting more than two years after stopping Keytruda. Finally, eight people experienced cancer progression.
Keytruda was safe and generally well tolerated. The most common side effects were anemia, fatigue, hypothyroidism, nausea, increased alkaline phosphate, decreased lymphocyte count and itching; 80% of these events were mild to moderate. A total of 10 severe or life-threatening adverse events were observed, mostly related to cancer.
One concern with checkpoint inhibitors is that in addition to restoring immune responses against cancer, they can unleash the immune system more broadly, leading to inflammation of healthy organs. In this study, 14 people developed immune-related events of clinical interest. A 61-year-old man with a history of both KS and NHL died from Castleman’s disease, a lymphoproliferative disorder linked to KS-associated herpesvirus, but this was not seen in any of the other people with KS or NHL.
“Our conclusion is that anti–PD-1 therapy is appropriate for cancer patients with well-controlled HIV and that patients with HIV and cancer can be treated with the drug and should be included in future immunotherapy studies,” Uldrick said in a Fred Hutch press release.
Imfinzi
In the second study, María González-Cao, MD, PhD, of Instituto Oncológico Dr. Rosell in Barcelona, and colleagues evaluated the safety and feasibility of Imfinzi for people with HIV.
The Phase II DURVAST trial enrolled 20 HIV-positive people with advanced solid tumors at 18 hospitals in Spain. Sixteen were men, and the median age was 54. People with a history of injection drug use, gay men and heterosexuals were all well represented. At study entry they had undetectable viral load and all but one had a CD4 count over 200, including 55% with more than 350 cells. People with hepatitis B or C or tuberculosis were excluded. A majority (70%) were using HIV integrase inhibitors, which have few interactions with other medications.
Fourteen had non-small-cell lung cancer, one had small-cell lung cancer, two each had melanoma and anal cancer and one had bladder cancer. One in four were starting first-line cancer treatment, while the rest were on their second to fourth treatment attempts.
Participants in this open-label study were treated with Imfinzi at the recommended dose of 1,500 milligrams every four weeks until disease progression or unacceptable toxicity. They remained on standard-of-care antiretroviral therapy during the study. Again, viral load remained suppressed and CD4 counts stayed about the same.
Four people (20%) experienced partial tumor shrinkage and five others (25%) had stable disease, González-Cao reported. Just over half (55%) experienced disease progression. At the time of the analysis, nine people remained on treatment. The median duration of response was 6.5 months, but the maximum duration exceeded 17 months. The median overall survival was 9.2 months, and the median progression-free survival was just 2.4 months. However, all four people who tested positive for the PD-L1 protein in their tumors were still alive.
Imfinzi, too, was safe and well tolerated. Most people experienced mild or moderate side effects, but only two had severe or life-threatening adverse events.
Taken together, these prospective studies focusing on people living with HIV show that PD-1/PD-L1 checkpoint inhibitors are safe for this population, with response rates and adverse event profiles similar to those seen in HIV-negative people.
Click here to read the Keytruda study in JAMA Oncology.
Click here to read the Imfinzi ASCO study abstract.
Click here to learn about checkpoint inhibitors in HIV cure research.






Comments
Comments