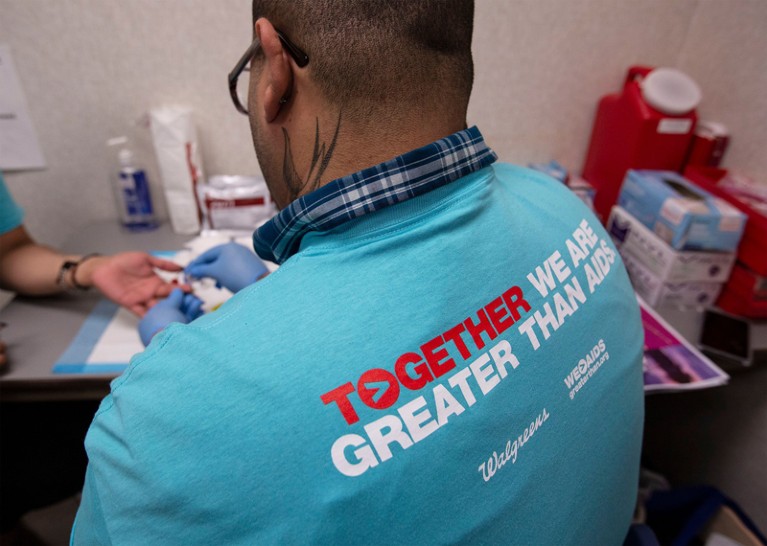
Increased HIV testing for people at high risk is part of a proposed strategy to stop HIV transmission in the United States by 2030.Credit: John Konstantaras/AP/Shutterstock
For the past two years, HIV advocacy groups have had little to like about US President Donald Trump’s administration. Trump has worked to reduce access to health-care programmes, threatened to cut funding to the global President’s Plan for Emergency AIDS Relief (PEPFAR), and stigmatized some communities at high risk. So it is little surprise that his 5 February pledge to end the HIV epidemic in the United States by 2030 has been met with some scepticism.
The effort is of course welcome and sorely needed: more than 1 million people in the United States have HIV, and 14% of them don’t know they are infected. And it’s reassuring to see that the programme is being headed by established leaders in the HIV field, including immunologist Anthony Fauci, director of the US National Institute of Allergy and Infectious Diseases (NIAID), and virologist Robert Redfield, director of the US Centers for Disease Control and Prevention (CDC).
Their approach is sound. It draws inspiration from global strategies to tackle the epidemic, such as the 90-90-90 programme of the Joint United Nations Programme on HIV/AIDS, which aims to reduce HIV infections through evidence-based action. Plans for the US programme include ramping up testing of people at high risk of HIV infection, offer these people prophylactic drugs that can reduce the risk of contracting HIV by 95%, and immediately starting those who test positive on antiretroviral treatments. (The administration has yet to say how much funding it will provide.)
It’s also encouraging that Fauci has said NIAID will fund studies to look at the best way to reach people at risk. The programme leaders are well aware of lessons from clinical trials in southern Africa showing that people need to feel not only that they have access to affordable HIV drugs, but also that health-care providers won’t stigmatize or criminalize them. “Stigma is the enemy of public health,” Redfield said in a press briefing on the programme last week.
And that is precisely where the project could run into trouble: Trump’s statements and policies have deeply undermined trust, and made health care harder to access, for those in some communities that are at highest risk of contracting HIV, including some people of colour, drug users, men who have sex with men, transgender people and those in poorer communities. Immigration crackdowns have left undocumented immigrants afraid to visit health clinics. The administration has opposed supervised injection sites, where drug users get clean needles to help them avoid contracting HIV and other infections. Last year, the US Department of Health and Human Services proposed a rule that would allow health-care providers to deny care on the basis of their moral or religious beliefs. Such a rule would mean that gay and transgender people could be turned away by some health clinics.
Meanwhile, some US policies abroad undermine public and reproductive health, weakening international efforts to prevent and treat HIV. The country’s ‘global gag rule’, put in place most recently by the Trump administration, cuts funding to foreign organizations providing reproductive health care if they so much as advise on terminating unwanted pregnancies. Yet reproductive-health clinics are key providers of HIV counselling, testing and care. Two major providers of family-planning services globally have now lost their US grants.
Eradicating HIV transmission in the United States is an exciting and achievable goal, and an opportunity for the country to lead the world in infectious-disease research and public health. That it is even possible shows how far HIV research and prevention have advanced in recent years. But delivering on it will require more than new drugs. It will take a major change in attitude and policies towards the people most affected by the disease.

 Scientists kick the tyres on Trump’s plan to tackle HIV
Scientists kick the tyres on Trump’s plan to tackle HIV
 How to beat HIV
How to beat HIV
 South Africa ushers in a new era for HIV
South Africa ushers in a new era for HIV







